Reporting
-
The State Regulatory Guidance (All Plan letters) responsibilities include, but are not limited to:
- DHCS All Plan Letter (APL) and Policy Letter (PL) Applicable Notices
- DHCS All Plan Letter (APL) and Policy Letter (PL) - Non-Applicable Notices
- Submits proof of APL and PL compliance documents to DHCS
-
The Organization Risk Assessment responsibilities include, but are not limited to:
- Review of new potential risks with assigned accountable business owners
- Provide final data set to senior executive team for implementation of agreed upon interventions
-
The Regulatory Audit Process responsibilities include, but are not limited to:
- Creation of audit folders
- Tracking of documents/universe and requests received from the auditor and distributed to the business owners
- Audit Readiness Questionnaires
-
The Regulatory Routine Reporting responsibilities include, but are not limited to:
- Maintaining calendar for all regulatory compliance
- Tracking timeliness of business owner’s submissions and attestation
Monitoring
Continuous monitoring allows a health plan to quickly and easily keep its finger on the pulse of the delegates’ performance to identify potential risks or issues before they become major problems. This will help ensure compliance with needed regulations through the health plan’s ability to:
- Expedite feedback processes to mitigate operational and enterprise risks
- Utilize streamlined reporting processes to automate reviews and highlight elements that are approaching identified tolerances
- Track findings, recommendations and corrective action plans, as well as trends over time, to quickly compare delegates and prepare for renegotiation when the time comes
Audit and CAP
Auditing delegated entities is essential for maintaining good governance, managing risk and ensuring compliance within an organization. Health plans can now efficiently oversee audits and perform file reviews of their delegated entities and vendors and maintain a system-wide overview of all compliance activities:
- Deliver real-time audit results
- Lower audit backlog, efforts and timelines
- Help health plans with pre- and post-delegation audits of all areas of delegation
- Create and manage Corrective Action Plans (CAP) for all audits that produce findings
Pre-delegation audit
The pre-delegation audit process involves a comprehensive review of the proposed delegates’ policies, procedures, and systems, as well as an assessment of their compliance with relevant technical and operational standards. The audit may also include a review of their financial stability and management structure. Our module helps guide the process through:
- Facility Site Review audits
- Medical Record Review audits
- Credentialing Audits Pre- and Annual re-certification
- Utilization Management audits including Quality Management (QM) audits
- Special Needs Plan (SNP) audits
Delegation repository
Centralized database of your various delegate or vendor information, allowing health plans to easily track and manage relationships with its FDRs.
AI Reshapes How U.S. Healthcare Payer CIOs Do Business
Generative AI for payers is no longer emerging; it’s accelerating transformation across compliance, operations, and member services.
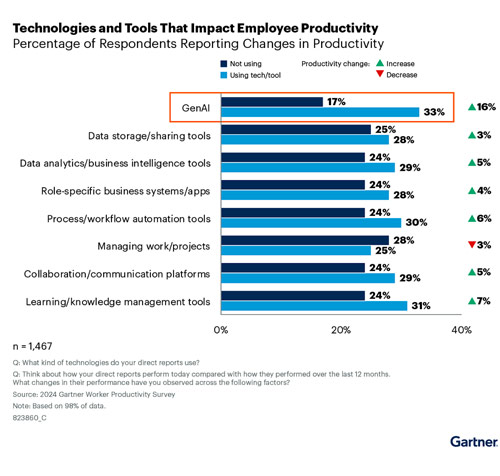
Gartner predicts, “By 2027, GenAI solutions will reduce administrative cost by 30% for most health insurers with more than one million members.”
Why this Gartner® report matters for healthcare payers
Healthcare payers today are under mounting pressure, rising administrative costs, evolving compliance mandates, and growing demand for operational efficiency. In this environment, Generative AI for payers is no longer optional, it’s a strategic necessity.
This Gartner report offers strategic insights into how Generative AI for payers and AI-powered automation are reshaping core functions like compliance, claims processing, and legacy system modernization.
Inside the report, you’ll discover:
- How AI and Generative AI are transforming payer operations and regulatory compliance
- Why 25% of payer legacy applications will be replaced by 2027, driven by rapid AI adoption and the shift to industry cloud platforms
- How AI automation can help lower Medical Loss Ratio (MLR) and reduce administrative burden
- Practical strategies to future-proof your health plan with scalable, AI-ready compliance solutions
Download the Gartner® report today to explore how digital transformation, regulatory readiness, and Generative AI will define the future of healthcare payers.
Access Gartner® Report
Disclaimer:
Gartner, Predicts 2025: AI Reshapes How U.S. Healthcare Payer CIOs Do Business, 16 January 2025, Faith Adams, et. Al.
GARTNER is a registered trademark and service mark of Gartner, Inc. and/or its affiliates in the U.S. and internationally and is used herein with permission. All rights reserved.
This graphic was published by Gartner, Inc. as part of a larger research document and should be evaluated in the context of the entire document. The Gartner document is available upon request from Inovaare.