Markets Served
Explore compliance solutions for Medicare, Medicaid, MMP, PBM and Commercial Health plans
Free eBook- From Algorithms to Outcomes: AI Integration in Health Plan Operations

Explore compliance solutions for Medicare, Medicaid, MMP, PBM and Commercial Health plans
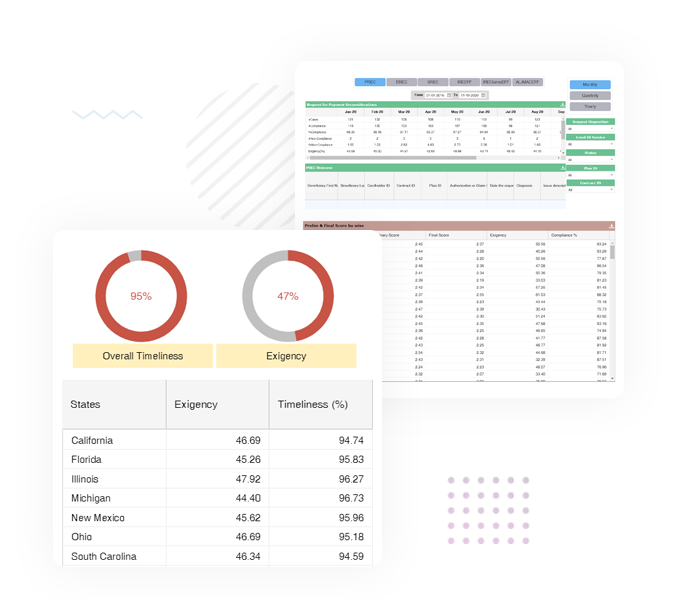
Inovaare's software-as-a-service (SaaS) platform delivers automated compliance solutions that enhance the member experience while lowering operating costs. Some of the largest health plans in the United States choose to partner with Inovaare to serve their Medicare, Medicare Advantage, Medicaid and MMP members as well as their commercial and third-party pharmacy benefit management (PBM) requirements. Designed by compliance experts with over 125 years of combined compliance experience, Inovaare's industry leading SaaS solutions help health plans gain a 360-degree view of their members while streamlining workflows and supporting quality. By harnessing disparate data across the entire enterprise, Inovaare empowers health plans to consistently maintain real-time compliance with federal and state regulatory bodies.



Medicare Advantage and Medicare Advantage Prescription Drug (MA/MAPD) plans face a unique set of regulatory challenges, forcing them to optimize administrative processes that comply with CMS requirements. Payer organizations are beginning to realize the importance of implementing automation software for appeals and grievances, universe management and regulatory compliance. Inovaare’s integrated platform empowers Medicare payers to: centralize MA/MAPD program requirements, automate CMS compliance processes and monitor compliance initiatives in real time.

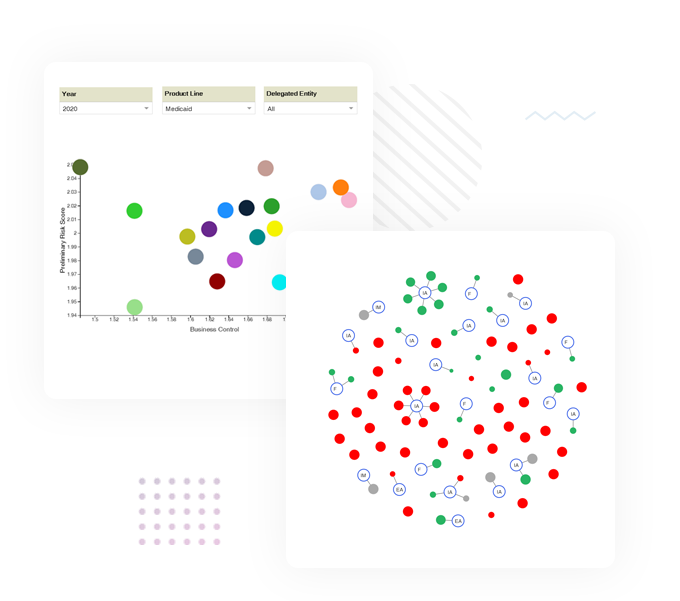
To be at the top of the Medicaid segment, payer plans must reduce operational inefficiencies, especially since Medicaid program administration is plagued by rampant insurance fraud and abuse. Detecting and deterring these criminal elements form the core of quality compliance audit tools.
Inovaare’s suite of comprehensive solutions for Medicaid providers addresses: appeals and grievances, universe management and regulatory compliance.
Inovaare supports Medicaid providers, including hospitals, to navigate the complex maze of Medicaid audit processes. Inovaare’s audit solution for Medicaid compliance helps payer plans to investigate suspicious provider activity, allowing them to quickly recover illegitimate claims, if processed, and track provider compliance with Medicaid program statutes.
To successfully move the needle in member experience, commercial health plans must improve member care and promote their unique selling proposition. This will empower them to compete in a cluttered marketplace.
Backed by over 125 years of leadership experience within the commercial health plan industry, Inovaare possesses unparalleled understanding of the challenges within the environment. Some of the largest commercial health plans in the United States trust Inovaare to guide them regarding unique contracting rules to help them provide better member service, improve provider engagement and promote enterprise-wide compliance.
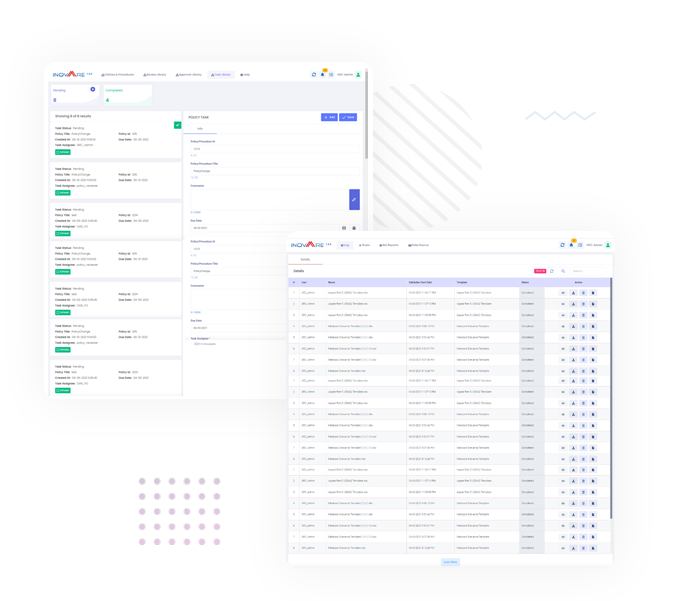
Based on recent finding from audits, the CMS increased oversight on pharmacy benefit management (PBM) operation. PBMs process a large volume of transactions and are responsible for complying with CMS and state regulations, as well as service-level agreement requirements of their clients. Inovaare’s next-generation cloud platform provides multiple solutions to address compliance and quality management requirements of PBMs and pharmacy operations.