Reporting
-
The State Regulatory Guidance (All Plan letters) responsibilities include, but are not limited to:
- DHCS All Plan Letter (APL) and Policy Letter (PL) Applicable Notices
- DHCS All Plan Letter (APL) and Policy Letter (PL) - Non-Applicable Notices
- Submits proof of APL and PL compliance documents to DHCS
-
The Organization Risk Assessment responsibilities include, but are not limited to:
- Review of new potential risks with assigned accountable business owners
- Provide final data set to senior executive team for implementation of agreed upon interventions
-
The Regulatory Audit Process responsibilities include, but are not limited to:
- Creation of audit folders
- Tracking of documents/universe and requests received from the auditor and distributed to the business owners
- Audit Readiness Questionnaires
-
The Regulatory Routine Reporting responsibilities include, but are not limited to:
- Maintaining calendar for all regulatory compliance
- Tracking timeliness of business owner’s submissions and attestation
Monitoring
Continuous monitoring allows a health plan to quickly and easily keep its finger on the pulse of the delegates’ performance to identify potential risks or issues before they become major problems. This will help ensure compliance with needed regulations through the health plan’s ability to:
- Expedite feedback processes to mitigate operational and enterprise risks
- Utilize streamlined reporting processes to automate reviews and highlight elements that are approaching identified tolerances
- Track findings, recommendations and corrective action plans, as well as trends over time, to quickly compare delegates and prepare for renegotiation when the time comes
Audit and CAP
Auditing delegated entities is essential for maintaining good governance, managing risk and ensuring compliance within an organization. Health plans can now efficiently oversee audits and perform file reviews of their delegated entities and vendors and maintain a system-wide overview of all compliance activities:
- Deliver real-time audit results
- Lower audit backlog, efforts and timelines
- Help health plans with pre- and post-delegation audits of all areas of delegation
- Create and manage Corrective Action Plans (CAP) for all audits that produce findings
Pre-delegation audit
The pre-delegation audit process involves a comprehensive review of the proposed delegates’ policies, procedures, and systems, as well as an assessment of their compliance with relevant technical and operational standards. The audit may also include a review of their financial stability and management structure. Our module helps guide the process through:
- Facility Site Review audits
- Medical Record Review audits
- Credentialing Audits Pre- and Annual re-certification
- Utilization Management audits including Quality Management (QM) audits
- Special Needs Plan (SNP) audits
Delegation repository
Centralized database of your various delegate or vendor information, allowing health plans to easily track and manage relationships with its FDRs.

Healthcare Payer Solutions
Healthcare Payer Solutions software for Medicare, Medicaid, MMP, Marketplace & Commercial Plans
Inovaare transforms complex compliance processes by designing configurable solutions so healthcare organizations can collect real-time data across internal and external departments, creating one compliance management system. Inovaare’s comprehensive suite of HIPAA-compliant software solutions and HITRUST platform features best-practice regulatory processes to help healthcare organizations efficiently meet their unique business requirements, sustain audit readiness, reduce non-compliance risks and lower overall operating costs.
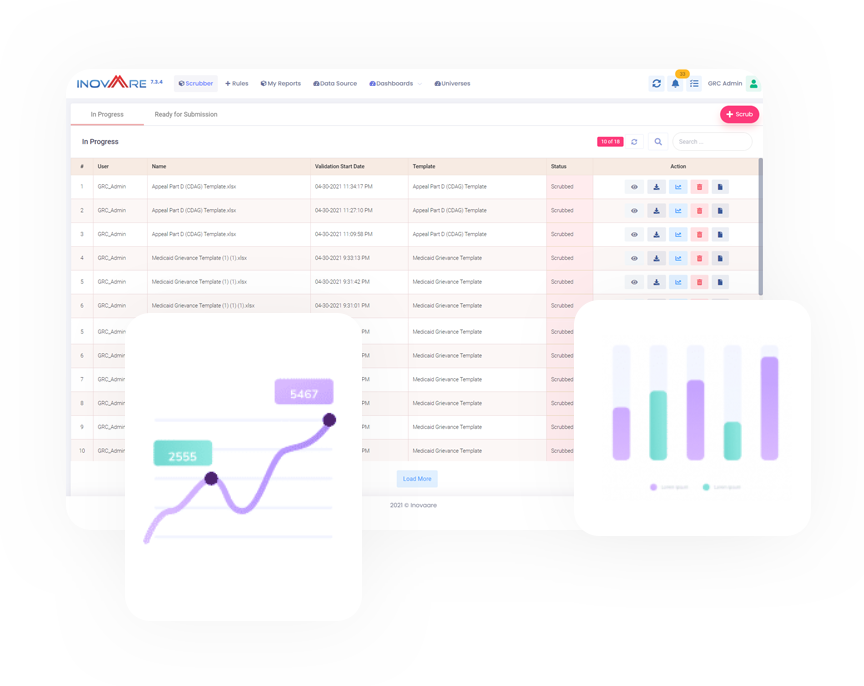
Introducing Universe Scrubber
Discover how to validate your
CMS universes within minutes
Health Plan Solutions to Sustain
Continuous Compliance
-
Appeals & Grievances
Appeals and grievances system with built-in compliance, workforce management and one-click universes
-
Audit Readiness
CMS universe management system for one-click universe generation and on-demand scrubbing of all universe tables for issue identification within minutes
-
Risk & Compliance
The CMS compliance module aligns with the latest CMS updates (i.e., HPMS) and helps plans create accurate risk assessments, manage corrective action plans (CAPs) and assign delegated tasks.
-
Data Warehouse
Centralized data repository for on-demand analytics and reporting through user-friendly, scalable interfaces that require minimal administration.
-
Reporting & Analytics
Business intelligence system with advanced reporting and analytics as well as ad hoc report and dashboard generation
-
CRM Member/ Provider
-
Appeals & Grievances
-
Audit Readiness
-
Risk & Compliance
-
Data Warehouse
-
Reporting & Analytics
-
CRM Member/Provider
Customer Relationship Management system exclusively focused on the operational and regulatory needs of health plan
-
Appeals & Grievances
Appeals and grievances system with built-in compliance, workforce management and one-click universes
-
Audit Readiness
CMS universe management system for one-click universe generation and on-demand scrubbing of all universe tables for issue identification within minutes
-
Risk & Compliance
The CMS compliance module aligns with the latest CMS updates (i.e., HPMS) and helps plans create accurate risk assessments, manage corrective action plans (CAPs) and assign delegated tasks.
-
Data Warehouse
Centralized data repository for on-demand analytics and reporting through user-friendly, scalable interfaces that require minimal administration.
-
Reporting & Analytics
Business intelligence system with advanced reporting and analytics as well as ad hoc report and dashboard generation
Improve Member Experiences
Ensure Faster Issue Resolution
Achieve Continuous Audit Readiness
Mitigate Risk for Better Operational Health
Make Better Decisions with Real-time Reports
Appeals and Grievances
Resolve the disconnect between multiple legacy systems to effectively engage members at every touchpoint in real time.
- Adhere to appeals and grievances compliance deadlines and requirements
- Monitor changes at each state of the complaint process
- Track and trend sales allegations outcomes
Audit & Monitoring
Efficiently audit and monitor compliance readiness by centralizing and automating critical processes.
- View audits and monitor process data in real time
- Track findings, recommendations and action plans
- Generate on-demand reports and analytics

Risk Management
Confidently guide health plans to manage risks relevant to their businesses with real-time data.
- View audits and monitor process data in real time
- Track findings, recommendations and action plans
- Generate on-demand reports and analytics

Delegation Oversight
Inovaare’s Delegation Oversight software suite, a cloud-based automation and workflow solution, helps health plans to:
- Deliver real-time audit statuses
- Lower audit backlog, efforts and timelines
- Conduct efficient pre- and post-delegation audits
Usher
Powered by a state-of-the-art Large Language Model (LLM) Deep Learning engine, Usher offers an unparalleled regulatory and policy compliance experience. To date, healthcare organizations have been able to achieve:
- Up to 80% reduction in searching for data
- Up to 60% increase in compliance performance
- Up to 30% increase in overall productivity
Inovaare Platform
Centralize critical data to meet government healthcare programs and commercial health-plan compliance requirements.
- Achieve compliance program effectiveness (CPE) objectives
- Ensure CMS Program Audit compliance
- Generate universes for Medicare, Medicaid and Commercial plans with the touch of a button


Inovaare is proudly powered by WordPress
